Plastic muscles and silicon senses blur the line between man and
machine.
 BY MIKE FILLON
BY MIKE FILLON
Illustration by Danilo
Ducak
In
a cluttered lab at the University of New Mexico, a replica of a human
skeleton slowly–very slowly–pedals an exercise bicycle. This is no parlor trick.
Myster Bony, as he's called, is moving the pedals
with artificial muscles powered by a battery.
It's
been 40 years since Swedish engineer Arne Larsson received the first fully
implanted cardiac pacemaker at the Karolinska Institute in Stockholm. Since
then, researchers throughout the world have looked for ways to improve people's
lives with artificial, bionic devices.
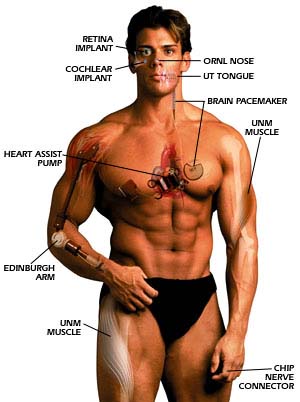
Their efforts
have produced smaller and smaller pacemakers, devices that help deaf children
hear and implantable pumps that carry the load for diseased hearts until
suitable human transplants can be found.
As for the
future, it looks decidedly more natural than the cyborg technology envisioned at
the dawn of the bionic age. Take Myster Bony. His muscles are made of materials
called ionic polymer metal composites (IPMCs) that respond to electricity with
elasticity and responsiveness similar to those shown by human muscles. The
materials were developed by a team led by Mohsen Shahinpoor, director of the
Artificial Muscle Research Institute (AMRI) at the University of New Mexico
(UNM).
Strips of these composites can bend and flap
dramatically when an electric current is applied. In this sense they are
large-motion actuators–they can move and exert force. Conversely, when a strip
is bent, voltage is produced across its thickness, allowing the strip to behave
like a sensor that can determine a given level of force and motion. These two
abilities–to move and to provide feedback– drive Myster Bony on his exercise
bicycle. All it takes is a power supply.
Another type of
artificial muscle being developed at AMRI is made of a synthetic fiber that has
been baked and boiled in a chemical solution. The treatment imparts strength and
gives the fabric elasticity that varies in the presence of an electric current.
The result: materials that can expand and contract just like living tissue.
Researchers envision a synthetic muscle that could
translate electrical impulses from the nervous system into motion. However, that
goal is still a long way off. In the short term, Shahinpoor believes artificial
muscles could be used to boost the strength of ailing hearts, eliminating some
heart transplants. He also imagines exoskeletons for disabled patients or
astronauts, artificial larynxes, and sensors for diagnosing spinal-cord
injuries. Eventually, his synthetic muscles could be attached to artificial
tendons, which recently have been approved by the Food and Drug Administration
for use in human patients.
A Real Bionic Arm
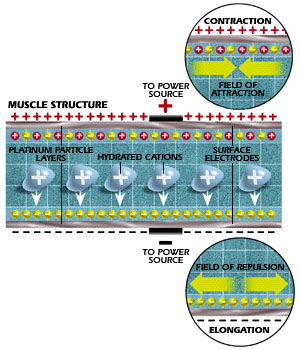 |
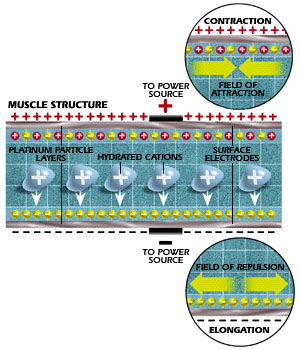
| In Myster Bony (right), a flow of
current through the artificial muscle causes the material to contract
(top) or elongate (bottom). Electrical change within the material also
provides feedback for control circuits that tell muscles how to
move. |
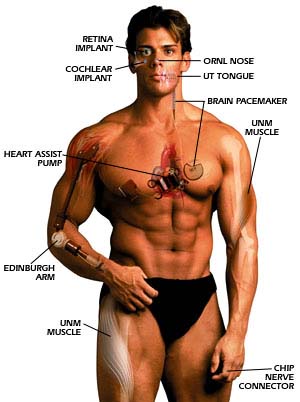
Artificial muscles aren't the only
electromechanical tools being developed to facilitate human movement. This past
summer, Campbell Aird, a hotel owner in Scotland, received a bionic arm that had
been developed by the Prosthetics Research and Development Team at Princess
Margaret Rose Orthopedic Hospital in Edinburgh. The arm uses electronics for
control and power. Known as EMAS (Edinburgh Modular Arm System), the arm is
equipped with battery-powered motors and epicyclical gearboxes. It replaced the
prosthetic limb Aird had worn since his own right arm was amputated 16 years ago
as a result of cancer.
The motors in Aird's arm are
mounted inside lightweight, rigid tubes of carbon fiber. The gearboxes are
connected to a worm-and-wheel assembly that converts the mechanical power of the
gearbox into rotary motion. The smallest motors and gearboxes power fingers and
the thumb, while larger motors power the wrist, elbow and shoulder. The arm is
covered with lifelike silicone rubber.
David Gow,
head of the team that developed the device, says EMAS was the first prosthesis
to have a fully powered electrical shoulder. In previous artificial arms, power
had been limited to wrists, elbows and hands. The arm is powered by rechargeable
12-volt batteries.
Modern prostheses like Aird's new
arm have a wider range of motion than ever before and look more like the limbs
they're replacing. Take the case of 10-year-old Melissa Del Pozzo. Melissa was
born without a left hand and lower forearm. Recently, in tests at Rutgers
University in New Jersey, she was able to make electrical traces on a computer
screen by moving either a tendon or a muscle that would have been used to flex
her thumb, if she had one. A sensor attached to the skin just below Melissa's
elbow detected the slight movements and relayed them to the computer screen.
 |
| The Edinburgh bionic arm can replace
conventional "muscle-powered" artificial
arms. |
Melissa
will soon be outfitted with what just may be the first dexterous prosthesis. To
fit her with a hand and control apparatus, researchers at Rutgers' department of
biomedical engineering, in Piscataway, N.J., will fashion a silicone sleeve
equipped with pressure sensors inside. On top of the sleeve will sit a hard
plastic socket that serves as an exoskeleton on which to anchor the hand. The
hand itself is a commercial wooden product used on other prostheses. It is
fitted with electromagnets that move each of three fingers separately. When a
tendon moves, the sensor, which consists of a small diaphragm, emits a puff of
air that travels through a tube to a transducer. In turn, the transducer senses
the pressure and transmits a precise electric signal to the artificial hand.
William Craelius, the principal researcher and an
associate professor of biomedical engineering at Rutgers, decided to focus on a
tendon-actuated system because previous teams had found it difficult to isolate
the muscle groups that can move individual fingers. Eventually, the dexterous
prosthesis may allow amputees to do such previously impossible tasks as playing
musical instruments and typing.
Powering And Control
 |
| Heart assist pumps help patients live
at home while awaiting
transplants. |
Providing power to run bionic
implants and making connections to the brain's control system pose the two great
challenges for biomedical engineering.
In the
mid-1970s, Medronics, a leading medical engineering firm, was trying to develop
a nuclear-powered heart pacemaker. About the same time, engineers at Drexel
University in Philadelphia maintained a dog's heartbeat using pacemakers with a
fuel cell that ran on the electricity generated by chemical reactions between
the dog's body and a block of aluminum. Neither alternative energy source proved
practical. For now, and perhaps decades to come, batteries of all shapes and
sizes will figure large in the future of bionics.
As
for controlling movement, the ultimate goal is to tap into the nervous system.
Researchers at the University of Michigan (UM) Center for Neural Communication
Technology are attempting to do just that. Here, they've developed probes so
precise they can stimulate or detect signals from individual nerve cells. The
probes (right) are only about the size of the date stamped on a penny.
 |
| This probe solves one of the most
technically difficult tasks, making a physical connection between a living
nerve and electric
current. |
The
probes are made of precisely etched silicon substrates covered with thin
conductive films, and insulated above and below. The upper surface is patterned
using a dry etching process. Tiny openings on the upper surface of the probe
shank are inlaid with gold or iridium, which are compatible with nerve tissue.
These are the spots where man melds with machine.
With sponsorship from the National Institutes of
Health's Neural Prosthesis Program, the number of probe designs has grown and UM
has provided more than 1000 devices to investigators.
Bionic Eyes
One of the most dramatic
applications of bionics is the creation of artificial eyes. Artificial retinas,
in particular, are showing great promise. Researchers have long known that
damaged photoreceptors in the eye could be bypassed (see diagram on page 55). A
device that stimulated the retinal ganglion cells–connected to the optic
nerve–could transmit visual information to the brain. Now, a new technology
promises to replace the retina, allowing the blind to see.
Working jointly, researchers at North Carolina State
University, the University of North Carolina and Johns Hopkins University have
created the implantable Artificial Retina Component Chip (ARCC). The ARCC
consists of a silicon microchip embedded with photosensor cells and electrodes.
It would be implanted near the vision center of the retina. Light and images
entering the pupil would pass through the ARCC's front surface and strike
photosensors on the back of the chip. The photosensor array would convert the
image pattern of light and dark into electric impulses, much as a healthy eye's
rods and cones do. The impulses would stimulate nerves behind the retina,
sending the information to the brain.
 |
| One promising approach is to use a
camera to "simplify" the view of the world and transmit an
easier-to-decode signal to the sensor, which is implanted on the
retina. |
The device is not expected to produce full, clear
vision. Instead, it would allow the patient to perceive basic shapes, the
direction of movements, and the boundaries between contrasting objects.
Bionic Sounds
Cochlear transplant research has
been around since the 1950s. In essence, cochlear implants provide electrical
stimulation of the auditory nerve. The implant sends sound waves into the
auditory pathway after converting them into electrical energy. Today, in
addition to numerous research institutions developing bionic hearing devices,
several companies are already selling commercial products. Although there are
differences in each product, they all work essentially the same way.
Even in the profoundly deaf, at least one-third of
the 30,000 fibers that stimulate the auditory nerve survive and are responsive,
capable of transmitting to the brain's hearing center. Signals to this center
are triggered by the cochlear implant.
Unlike
hearing aids, which amplify sound, the cochlear implant–or bionic ear–trades in
electricity. Surgeons implant the device in the mastoid bone and inner ear
through an incision behind the ear. A small speech processor converts sound,
picked up by an external mike, into an electrical signal. The signal is fed
through the transmitter coil to the implanted receiver. Electrodes in the inner
ear bypass the damaged area of the ear and create a nerve impulse that
stimulates the auditory cortex of the brain.
Artificial cochleas will not benefit all deaf
people. Adults who have never heard are not suitable candidates, doctors say,
because the auditory part of their brains will not respond to the stimuli.
In an entirely different approach, Jonathan Spindel,
a biomedical engineer and assistant professor at the University of Virginia's
department of otolaryngology, is developing an implanted "invisible" magnetic
hearing aid. "Our tests to date have shown that the signals produced with our
magnetic hearing device are very nearly those of natural acoustic sound," says
Spindel.
 |
| The cochlea (inset) is filled with
hairlike structures that stimulate nerves. Naturally it is stimulated by
changes in air pressure. Here, it's artificially stimulated by the
implant. |
In this approach, the device captures sounds with
a miniature microphone implanted in the ear. After passing through a small
processing unit and an electromagnetic coil, both also implanted, amplified
vibrations would be sent to the inner ear via a tiny magnet attached to the
inner ear's round window, a thin membrane at one end of the cochlea. The magnet,
about as large as a pencil point, would send vibrations through the cochlea,
stimulating the thousands of hair cells used in normal hearing.
Spindel says an advantage of his approach is that
the device doesn't obstruct the normal hearing process. "Establishing a second
independent input pathway to the inner ear opens the possibility for using the
normal acoustic pathway and round window electromagnet simultaneously to
establish constructive and destructive sound patterns in the inner ear."
Also, since the new hearing device uses magnetic
rather than acoustic vibrations, feedback–a common problem in conventional
hearing aids–is eliminated.
Senses And Sensibilities
 |
| The nose is nature's own chemical
analysis system. ORNL's sensors and circuitry can differentiate among
odors. The circuitry hardware can be compressed onto a computer
chip. |
Unlike sight and hearing, scientists
know little about the human senses of smell and taste. Nevertheless, they have
been able to re-create these abilities. They try to mimic human noses by using
sensors that can detect a variety of volatile compounds.
For example, at the Oak Ridge National Laboratories
(ORNL), in Oak Ridge, Tenn., a "nose on a chip" is proving able to sniff out
mercury, carbon monoxide and other chemicals. It consists of an array of
minuscule sensors on one integrated circuit, with the electronics on a separate
one. By selectively coating the arrays with different chemicals, researchers can
customize the chip to detect virtually any odor.
At
the University of Texas (UT) in Austin, researchers have developed an electronic
tongue that mimics the human ability to detect sweet, sour, salty and bitter
tastes.
To do this, the team attached four different
chemical sensors to tiny beads made of polyethylene glycol and polystyrene. The
beads were then positioned in micromachined wells on a silicon wafer. The
sensors represent various combinations of the four different taste elements with
combinations of the colors red, green and blue. For example, when exposed to an
acidic "taste" one sensor turns yellow. It becomes purple when a basic mixture
is sensed.
 |
| Taste can be roughly duplicated with
UT's optoelectronic system. Different chemical properties cause sensing
beads in the silicon taste bud (left and middle) to change color.
Electronic circuitry expresses the color change as "taste." As on a real
tongue (left), different parts of the silicon tongue (right) are sensitive
to different compounds. |
Bionic noses and tongues are simply laboratory tools
at this time, and there are no plans to incorporate them into humans in the
future.
Not yet, at least.
Not Just Body Parts
Bionic devices are being
developed to do more than replace defective parts. Researchers are also using
them to fight illnesses.
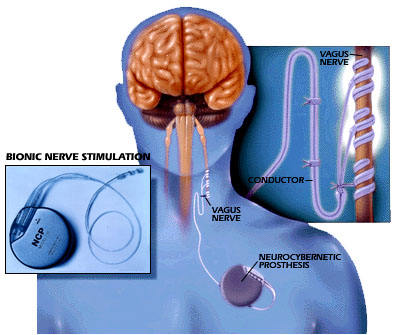
For instance, the
NeuroCybernetic Prosthesis (NCP) system is designed to provide relief for the
hundreds of thousands who currently suffer from debilitating epileptic seizures.
Recent research proves that vagus nerve stimulation
alters or modulates blood flow in areas of the brain where seizures are known to
start or spread. Acting as a "pacemaker for the brain," the NCP system,
manufactured by Cyberonics, delivers a unique therapy, called Vagus Nerve
Stimulation (VNS), to individuals unable to control their disorder using drug
therapy or surgery. This device, roughly the size of a pocket watch, is
implanted in the patient's chest with small wires leading to the vagus nerve in
the neck. The device sends precisely timed and measured electrical pulses to the
nerve, which controls the activity of several internal organs. It has been
proven to decrease or even eliminate seizures.
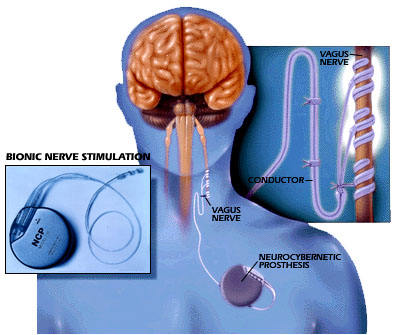 |
| A sensor detects a seizure before it
becomes pronounced and sends an electronic impulse to the vagus nerve.
This prevents the seizure from
escalating. |
With the technology to link man's nerves to
electronic circuits progressing rapidly, it is only a matter of time before our
brains can communicate with bionic devices. Then we will be at the threshold of
making a true "bionic man."


 BY MIKE FILLON
BY MIKE FILLON